We’ll now learn how Ferrara Candy Company boosts its agility as a manufacturer by expanding the use of analysis and proactive refinement in its data center operations by bringing more intelligence to IT infrastructure.
Stay with us to hear about unlocking the potential for end-to-end process and economic efficiency with Stefan Floyhar, Senior Manager of IT Infrastructure at Ferrara Candy Co. in Oakbrook Terrace, Illinois. The discussion is moderated by Dana Gardner, Principal Analyst at Interarbor Solutions.
Here are some excerpts:
Gardner: What
are the major reasons Ferrara Candy took a new approach in bringing added
intelligence to your servers and storage operations?
Floyhar: The
driving force behind utilizing intelligence at the infrastructure level specifically
was to alleviate the firefighting operations that we were constantly undergoing
with the old infrastructure.
Gardner: And
what sort of issues did that entail? What was the nature of the firefighting?
Floyhar: We
were constantly addressing infrastructure-related hardware failures, firmware issues,
and not having visibility into true growth factors. That included not knowing what’s
happening on the backend during an outage or from a problem with performance.
We had a lack of visibility into true real-time performance data and fully
scalable performance data.
Gardner: There’s
nothing worse than being caught up in reactive firefighting mode when you’re also
trying to be innovative, re-architect, and adjust to things like mergers and
growth. What were some of the business pressures that you were facing even as
you were trying to keep up with that old-fashioned mode of operations?
IT meets expanded candy demands
 |
| Floyhar |
Floyhar: We
have undergone a significant amount of growth in the last seven years -- going
from 125 virtual machines to 452, as of this morning. Those 452 virtual
machines are all application-driven and application-specific. As we continued
to grow, as we continued to merge and acquire other candy companies, that
growth exploded exponentially.
The merger with Ferrara Pan Candy,
and Farley’s and Sathers in 2012, for example, saw an initial growth
explosion. More recently, in 2017 and 2018, we were acquired by Ferrero. We
also acquired
Nestlé Confections USA, which has essentially doubled the business
overnight. The growth
is continuing at an exponential rate.
Gardner: The
old mode of IT operations just couldn’t keep up with that dynamic environment?
Floyhar: That
is correct, yes.
Gardner:
Ferrara Candy might not roll off the tongue for many people, but I bet they
have heard a lot of your major candy brands. Could you help people understand
how big and global you are as a confectionery manufacturer by letting us know
some of your major brands?
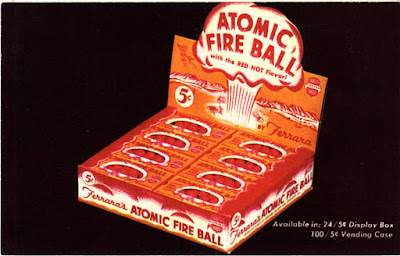
Floyhar: We
are the producers of Now
and Later, Lemonheads,
Boston
Baked Beans, Atomic
Fireballs, Bob’s Candy
Canes, and Trolli Gummies,
which is one of our major brands. We also recently acquired Crunch Bar, Butterfinger, 100 Grand, Laffy Taffy, and Willy Wonka brands,
among others.
We produce a little over 1 million
pounds of gummies per week, and we are currently utilizing 2.5 million square
feet of warehousing.
Gardner: Wow!
Some of those brands bring me way back. I mean, I was eating those when I was a
kid, so those are some age-old and favorite brands.
Let’s get back to the IT that supports
that volume and diversity of favorite confections. What were some of the major
drivers that brought you to a higher level of automation, intelligence, and
therefore being able to get on top of operations rather than trying to play catch
up?
Floyhar: We
have a very lean staff of engineers. That forced us to seek the next generation
of product, specifically around artificial intelligence
(AI) and machine learning
(ML). We absolutely needed that because we’re growing at this exponential
rate. We needed to take the focus off of infrastructure-related tasks and
leverage technology to manage and operate the application stack and get it up
to snuff. And so that was the major driving force for seeking AI [in our
operations and management].
Gardner: And
when you refer to AI you are not talking about helping your marketers better
factor which candy to bring into a region. You are talking about intelligence
inside of your IT operations, so AIOps, right?
Floyhar: Yes,
absolutely. So things like Hewlett Packard
Enterprise (HPE) InfoSight and some of the other providers with cloud-type
operations for failure metrics and growth perspectives. We needed somebody with
proven metrics. Proven technology was a huge factor in product determination.
Gardner: How
about storage
specifically? Was that something you targeted? It seems a lot of people
need to reinvent and modernize their storage and server infrastructure in
tandem and coordination.
Floyhar: Storage
was actually the driving factor for us. It’s what started the whole renovation
of IT within Ferrara. With our older storage, we were constantly suffering
bottlenecks with administrative tasks and in not having visibility into what
was going on.
During
that discovery process and research, HPE InfoSight really jumped off
the page at us. That level of AI, the proven track record, and being
able to produce data around my work loads.
Storage drove that need for
change. We looked at a lot of different storage area networks
(SANs) and providers, everything from HPE Nimble to Pure, VNX, Unity, Hitachi, …
insert major SAN provider here. We probably did six or so months’ worth of
research working with those vendors, doing proof of concepts (POCs) and looking
at different products to truly determine what was the best storage solution for
Ferrara.
During that discovery process,
during that research, HPE InfoSight really jumped off the page at us. That
level of AI, the proven track record, being able to produce data around my actual
work loads. I needed real-life examples, not a sales and marketing pitch.
By having a demo and seeing
that data being given that on the fly and on request was absolutely paramount
in making our decision.
Gardner: And,
of course, InfoSight, was a part of Nimble Storage and Nimble
became acquired by HPE. Now we are even seeing InfoSight technology being distributed
and integrated across HPE’s broad infrastructure offerings. Is InfoSight
something that you are happy to see extended to other areas of IT infrastructure?
Floyhar: Yes, ever
since we adopted the Nimble Storage solution I have been waiting for InfoSight
to be adopted elsewhere. Finally it’s been added across the ProLiant series of
servers. We are an HPE
ProLiant DL560 shop.
I am ultra-excited to see what
that level of AI brings for predictive failures monitoring, which is
essentially going to alleviate any downtime. Any time we can predict a failure,
it’s obviously better than being reactive, with a retroactive approach where
something fails and then we have to replace it.
Gardner: Stefan, how do you consume that proactive insight? What does InfoSight bring in terms of an operations interface? Or have you crafted a new process in your operations? How have you changed your culture to accommodate such a proactive stance? As you point out, being proactive is a fairly new way of avoiding failures and degraded performance.
Proactivity improves productivity
Floyhar: A lot
of things have changed with that proactivity. First, the support model, with the
automatic opening and closure of tickets with HPE support. The Nimble support
is absolutely fantastic. I don’t have to wait for something reactive at 2 am,
and then call HPE support. The SAN does it for me; InfoSight does it for me. It
automatically opens the ticket and an engineer calls me at the beginning of my
workday.
No longer are we getting
interrupted with those 2, 3, 4 am emergency calls because our monitoring
platform has notified us that, “Hey, a disk failed or looks like it’s going to
fail.” That, in turn, has led to a complete culture change within my team. It takes
us away from that firefighting, the constant, reactive methodologies of
maintaining traditional three-tier infrastructure and truly into leveraging AI and
the support behind it.
We are now able to turn the
corner from reactive to proactive, including on applications
redesign or re-work, or on tweaking performance improvements. We are taking
that proactive approach with the applications themselves, which has rolled even
further downhill to our end users and improved their productivity.
In the last six months, we
have received significant praise for the applications performance, based on
where it was three years ago compared with today. And, yes, part of that is
because of the back-end upgrades in the infrastructure platform, but also
because as we’ve been able to focus more on the applications administration
tasks and truly making it a more pleasant experience for our end users -- less
pain, less latency, just less issues.
Gardner: You
are a big SAP shop, so that improvement
extends across all of your operations, to your logistics and supply chain, for
example. How does having a stronger sense of confidence in your IT operations
give you benefits on business-level innovation?
Floyhar: As
you mentioned, we are a large SAP shop. We run any number of SAP-insert-acronym-here
systems. Being proactive on addressing some of the application issues has
honestly caused less downtime for the applications. We have seen into the four-
and five-9s (99.99-9 percent) uptime from an application availability
perspective.
We have been able to
proactively catch a number of issues, whether using HPE InfoSight or standard
notifications. We have been able to proactively catch a number of issues that
would have caused downtime, even as minimal as 30 minutes. But when you start
talking about an operation that runs 24x7, 360 days a year, and truly depends
on SAP to be the backbone, it’s the lifeblood of what we do on a business
operations basis.
So 30 minutes makes all the
difference on the production floor. Being able to turn that support corner has
absolutely been critical in our success.
Gardner: Let’s
go back to data. When it comes to having storage confidence, you can extend that
confidence across your data lifecycle. It's not just storage and accommodating
key mission-critical apps. You can start to modernize and gain efficiencies through
backup and recovery, and to making the right cache and de-dupe decisions.
What’s it been like to extend
your InfoSight-based intelligence culture into the full data lifecycle?
Sweet, simplified data backup and recovery
Floyhar: Our
backup and recovery has gotten significantly less complex -- and significantly
faster -- using Veeam with the storage API
and Nimble
snapshots. Our backup window went from about 22.5 hours a day, which was
less than ideal, obviously, down to less than 30 minutes for a lot of our
mission-critical systems.
We are talking about 8-10
terabytes of Microsoft
Exchange data, 8-10 terabytes of SAP data -- all being backed up, full
backups, in less than 60 minutes, using Veeam
with the storage API. Again, it’s transformed how much time and how much
effort we put into managing our backups.
Again, we have turned the
corner on managing our backups on an exception-basis. So now it’s only upon
failure. We have gained that much trust in the product and the back-end
infrastructure.
We
specifically watch for failure, and any time something comes up that's
what we address as opposed to watching everything 100 percent of the
time to make sure it's working.
We specifically watch for failure, and any time something comes up that’s what we address as opposed to watching everything 100 percent of the time to make sure that it’s all working. Outside of the backups, just every application has seen significant performance increases.
Gardner:
Thinking about the future, a lot of organizations are experimenting more with hybrid
cloud models and hybrid IT models. One of the things that holds them up from adoption
is not feeling confident about having insight, clarity, and transparency across
these different types of systems and architectures.
Does what HPE InfoSight and
similar technologies bring to the table give you more confidence to start
moving toward a hybrid model, or at least experimenting in that direction for
better performance in price and economic payback?
Headed to hybrid, invested in IoT
Floyhar: Yes,
absolutely, it does. We started to dabble into the cloud, and a mixed-hybrid
infrastructure a few years before Nimble came into play. We now have a
significantly larger cloud presence. And we were able to scale that cloud
presence easily specifically because of the data. With our growth trending, all
of the pieces involved with InfoSight, we were able to use that data to scale
out and know what it looks like from a storage perspective on Amazon Web Services (AWS).
We started with SAP HANA out in
the cloud, and now we’re utilizing some of that data on the back end. We are
able to size and scale significantly better than we ever could have in the past,
so it has actually opened up the door to adopting a bit more cloud architecture
for our infrastructure.
Gardner: And
looking to the other end from cloud, core, and data center, increasingly manufacturers
like yourselves -- and in large warehouse environments like you have
described -- the Internet
of Things (IoT) is becoming much more in demand. You can place sensors and
measure things in ways we didn’t dream of before.
Even though IoT generates
massive amounts of data -- and it’s even processing at the edge – have you
gained confidence to take these platform technologies in that direction, out to
the edge, and hope that you can gain end-to-end insights, from edge to core?
Floyhar: The executives
at our company have deemed that data is a necessity. We are a very data-driven
company. Manufacturers of our size are truly benefiting from IoT and that data.
For us, people say “big data” or insert-common-acronym-here. People process big
data, but nobody truly understands what that term means.
With our executives, we have gone
through the entire process and said, “Hey, you know what? We have actually
defined what big data means to Ferrara. We are going to utilize this data to
help drive leaner
manufacturing processes, to help drive higher-quality products out the door
every single time to achieve an industry standard of quality that quite frankly
has never been met before.”
We have very lofty goals for
utilizing this data to drive the manufacturing process. We are working with a
very large industrial automation company to assist us in utilizing IoT, not
quite edge computing yet, but we might get there in the next couple of years. Right
now we are truly adopting the IoT mentality around manufacturing.
And that is, as you mentioned,
a huge amount of data. But it is also a very exciting opportunity for Ferrara.
We make candy, right? We are not making cars, or tanks, or very expansive
computer systems. We are not doing that level of intricacy. We are just making
candy.
But to be able to leverage the machine data at almost every inch of the factory floor? If we could get that and utilize it to drive end-to-end process, efficiency, and manufacturing efficiencies? It not only helps us produce a better-quality product faster, it’s also environmentally conscious, because there will be less waste, if any waste at all.
The list of wonderful things
that comes out of this goes on and on. It really is an exciting opportunity. We
are trying to leverage that. The intelligent back-end storage and computer systems
are ultra-imperative to us for meeting those objectives.
Gardner: Any
words of advice for other organizations that are not as far ahead as you are
when it comes to going to all-flash and highly intelligent storage -- and then
extending that intelligence into an AIOps culture? With 20/20 hindsight, for
those organizations that would like to use more AIOps, who would like to get
more intelligence through something like HPE InfoSight, what advice can you
give them?
Floyhar: First
things first -- use it. For even small organizations, all the way up to the
largest of organizations, it may almost seem like, “Well, what is that data
really going to be used for?” I promise, if you use it, it is greatly
beneficial to your IT operations.
Historically
we would constantly be fighting infrastructure-related issues --
outages, performance bottlenecks, and so on. With the AI behind HPE
InfoSight, the AI makes all the difference. You don't have to fight that
fight when it becomes a problem because you nip it in the bud.
If you don't have it -- get
it. It’s very important. This is the future of technology. Using AI to
predictively analyze all of the data -- not just from your environment -- but
being able to take a conglomerate view of customer data and keep it together
and use predictive analytics – that truly does allow IT organizations to turn
the corner from reactive to proactive.
Historically we would
constantly be fighting infrastructure-related issues -- outages, performance
bottlenecks, and so on. With the AI behind HPE InfoSight, and other providers, including
cloud platforms, the AI makes all the difference. You don’t have to fight that fight
when it becomes a problem because you get to nip it in the bud.
Listen to the podcast. Find it on iTunes. Read a full transcript or download a copy. Sponsor: Hewlett Packard Enterprise.
You may also be
interested in:
- How Texmark Chemicals pursues analysis-rich, IoT-pervasive path to the ‘refinery of the future'
- How the composable approach to IT aligns automation and intelligence to overcome mounting complexity
- How HPC supports 'continuous integration of new ideas' for optimizing Formula 1 car design
- Want to manage your total cloud costs better? Emphasize the ‘Ops’ in DevOps, says Futurum analyst Daniel Newman
- A new Mastercard global payments model creates a template for an agile, secure, and compliant hybrid cloud
- Where the rubber meets the road: How users see the IT4IT standard building competitive business advantage
- IT kit sustainability: A business advantage and balm for the planet
- Industrial-strength wearables combine with collaboration cloud to bring anywhere expertise to intelligent-edge work
- How the data science profession is growing in value and impact across the business world